It’s 11:30 on a Friday night at San Jose Medical Center. In the operating room are the victims of an auto accident — a woman, seven months pregnant, and her five-year-old son. In the emergency department, 14 patients and their families fill the treatment rooms and waiting areas. Three of them are critically ill.
With the emergency staff and two surgical teams fully occupied, the supervisor is about to direct staff to temporarily divert new paramedic patient arrivals to other hospitals. Two of the three closest hospitals already are diverting patients due to overload. A few minutes later, paramedics radio the Medical Center. They just picked up a woman near one of the diverting hospitals. She is having a severe asthma attack. She needs attention quickly. Can the Medical Center take her?
Such scenes as the one described above were occurring with greater frequency at the San Jose Medical Center (SJMC) in the late 1980s. A hospital goes on temporary diversion status when it cannot safely accept more emergency patients because of insufficient staff, operating rooms, or beds. In San Jose, the proportion of time in which paramedic patients were diverted to other hospitals gradually increased from a monthly average of 5% in 1986 to 35% in 1990 (see “Paramedic Diversion Rate” graph). The increase in paramedic diversions was not confined to SJMC. Other hospitals were experiencing diversion rates ranging from 25-65%. The county-operated hospital, which had the heaviest emergency patient load, also had the highest diversion rate — more than 80% in early 1990.
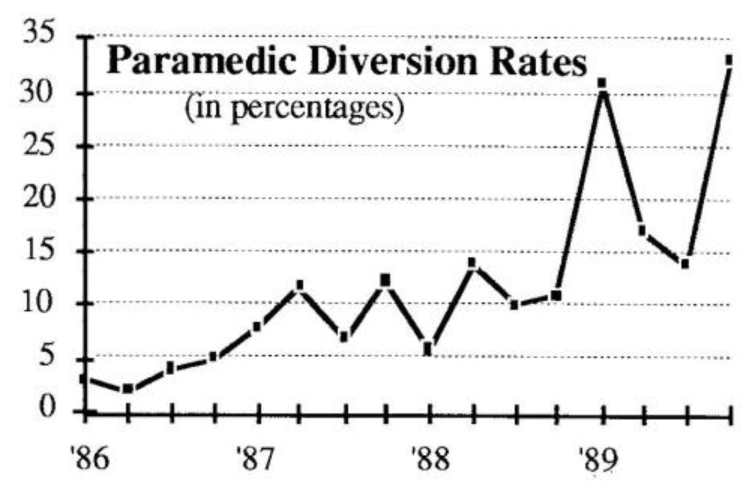
The growing diversion rates indicated a number of stresses in the San Jose community hospital system. Between 1986 and 1988, for example, the shift from scheduled admissions to emergency admissions grew at a six percent average annual rate. During the same period, demand for hospital critical care services increased by four percent per year.
While demand for these services was growing, actual hospital capacity for critical care services remained fixed or declined. The demand for emergency-origin patients had grown faster than capacity, and the community-wide emergency medical system was becoming dysfunctional.
Decreased Quality of Service
The community incurs tremendous costs when its emergency service system has such frequent closures. When paramedic diversion rates increase, service quality suffers because of the longer time delays as paramedics “circle” around looking for an open hospital. Not only is treatment delayed, but the paramedics are distracted from their patient care duties while they spend time on the radio trying to find an open hospital.
Since already overloaded hospitals are more likely to accept patients whose conditions arc less severe, medical conditions are more likely to be misrepresented in the field. And, as the paramedics’ frustration mounts, the number of patients brought in with no prior alert — and therefore no hospital preparation — increases. These unexpected arrivals only add to the overload and lengthen the already long wait.
Systems Thinking Approach
San Jose Medical Center was particularly concerned with the growing problem of paramedic diversions since it has a history of commitment to emergency medical service. SJMC operates the busiest of three designated trauma centers in the county, and its location near the center of the population and several freeways makes it a leading hospital for paramedic patients. But as the number of diverted patients from other zones had grown, SJMC’s capacity to treat patients from its own market was greatly reduced. The result was frequent patient backlogs at various points within the Medical Center.
To address this problem, our team of department directors and executives at SJMC applied a systems thinking approach to better understand and address the growing unavailability of Medical Center capacity for emergency patients.
The key questions we addressed were:
- Where are the highest-leverage points for improving our capacity to serve emergency patients?
- What will it take (resources, structural changes) to implement those strategies?
- How much of the gap between current diversion rates (35%) and our short-term goal of 12% can be reduced by internal interventions?
(Editor’s note: Readers may want to try their hand at answering the above questions and perhaps identify analogous “emergency service” situations in their own organizations.)
To address the problem of capacity constraints and paramedic diversions, the SJMC project team began by gathering subjective data. Our goal was to collect team members’ “conventional wisdom” (mental models) about the emergency care system — its problems, the causes, and possible solutions. We then identified measurable outcomes SJMC wanted to attain, compared our actual performance with the desired performance, and calculated the gap we needed to close. To develop a preliminary understanding of the potential leverage points within the system, we developed a conceptual model which described how the system works in terms of typical operational situations.
Domino Effect
When we looked more closely at current operations of individual hospitals, we found that when the county-operated hospital diverted paramedic patients, a nearby community hospital would also go to diversion status to avoid becoming overloaded and receiving “undesirable” emergency patients. This behavior worsened the impact on other hospitals, particularly SJMC, which would then receive both hospitals’ overflow (see “Domino Effect of Paramedic Diversions” graph). The overflow would cause SJMC to go into diversion status more rapidly, causing diverted patients to flow to the next hospital, and so on. In effect, a primary cause of the overall paramedic diversion problem was the ripple effects of capacity limitations at one hospital.
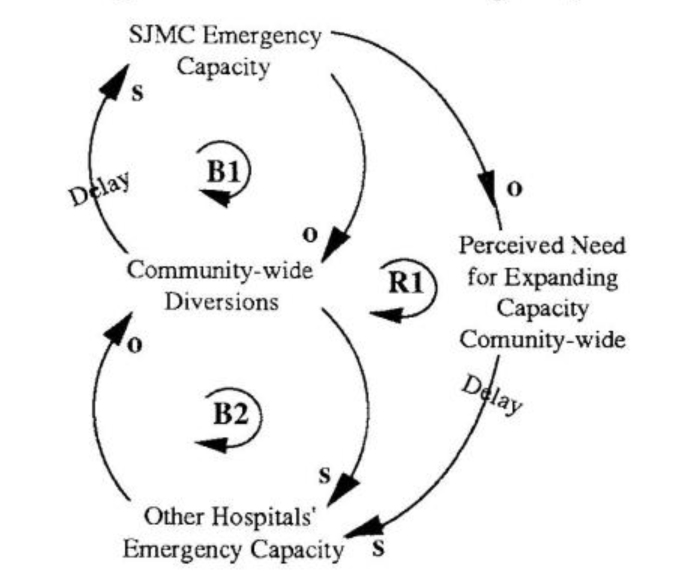
Our initial project goal had been to reduce SJMC’s diversion rate, because diversions meant not meeting one of our most basic responsibilities — to provide emergency medical care to our community. But now that we understood the broader community-wide system, we realized that the more SJMC increased its capacity in order to prevent going to diversion status, the more patients we received from other hospital diversions. The result was an even greater strain on capacity, and more SJMC diversions.
Shifting the Burden Structure
As long as other hospitals were diverting a significant proportion of paramedic patients, stepping up capacity at SJMC would simply result in our seeing more and more diverted patients until we exhausted our added capacity (loop BI in “Shifting the Burden of Emergency Care”). In addition, our efforts to increase internal capacity were unintentionally alleviating pressure on the system to resolve the broader problem — an overall lack of emergency capacity at the community’s hospitals (loop B2).
Domino Effect of Paramedic Diversions
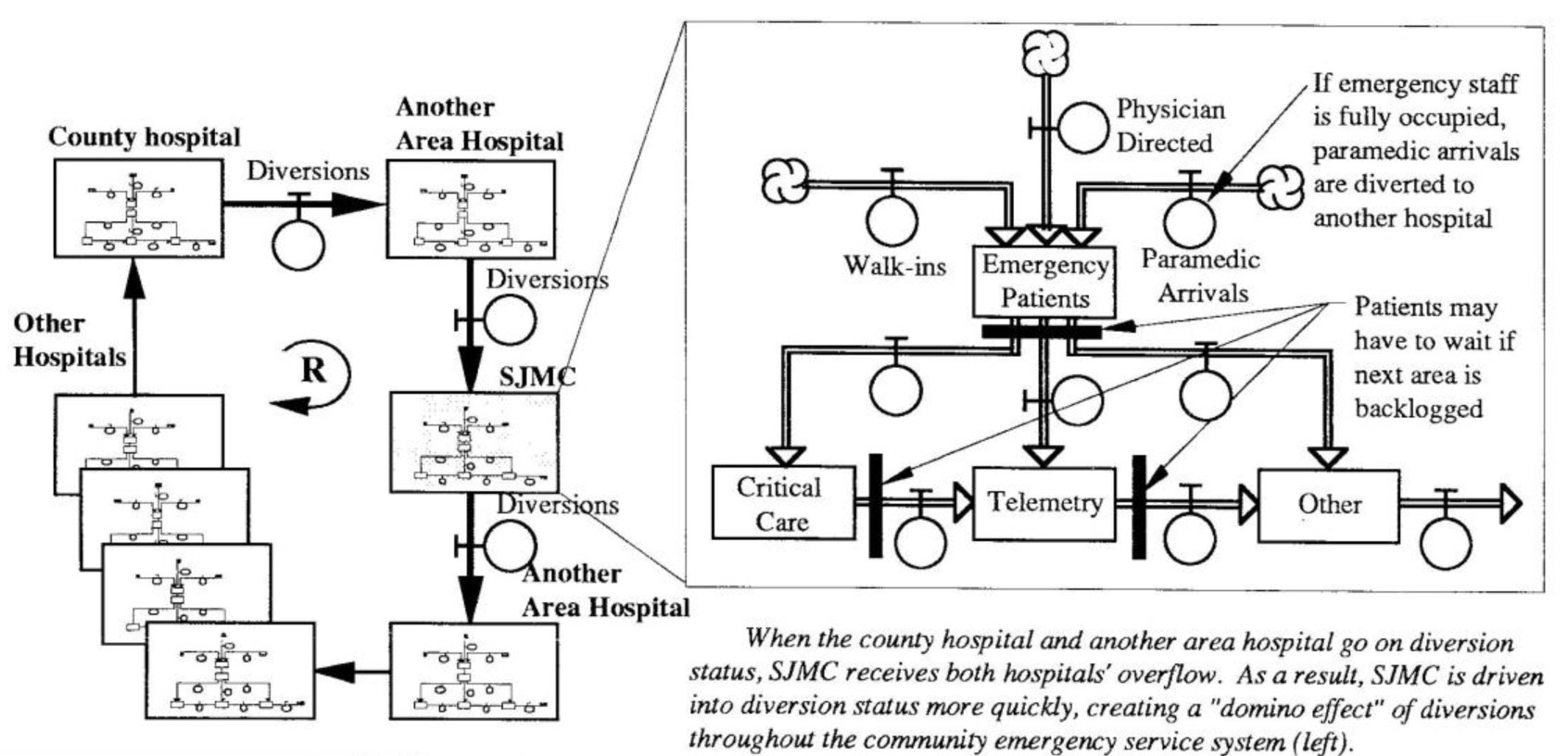
When the county hospital and another area hospital go on diversion status, SJMC receives both hospitals’ overflow. As a result, SJMC is driven into diversion status more quickly, creating a “domino effect” of diversions throughout the community emergency service system (left).
We began to realize that the fundamental solution to the community-wide problem was a public policy intervention that would ensure that all hospitals maintain a generally “open” emergency medical service. That way, no one hospital or group of hospitals could disrupt the entire system.
Ironically, our previous capacity expansion efforts had masked the need for a public policy intervention (loop RI), because the burden of providing adequate emergency service capacity had been shifted to SJMC. We concluded that the single, highest-leverage solution to the problem was to implement public policy that would require all hospitals in the emergency medical care system to receive paramedic patients (except in rare instances).
Reframing the Problem
In light of the above insights, we revised our definition of the problem. It was now evident that external action was likely to have the greatest impact on SJMC’s diversion rate. Internally, however, several questions still remained: If the community-wide diversion rate were reduced to a reasonable level, would SJMC continue to have an emergency capacity problem? If new capacity were needed, which internal interventions will produce the greatest yield in terms of freeing up capacity and enabling more patients to be served? In order to address such questions, we developed a computer model.
Our initial work had provided a great deal of insight into the diversion/ capacity issue; the computer model now allowed us to leverage our understanding even further. If the initial phase took us from an understanding level of one to five, using the computer allowed us to leap to a level of nine. The model enabled us to test out specific policy recommendations, compare the results with other policies, and access which ones were more desirable — all without risking a single patient’s life or a physician’s career.
We tested alternative strategies for improving internal capacity such as adding staff, adding beds or operating rooms, altering protocol for paramedic diversions, improving system productivity, and moving patient bed locations. We then measured various outcomes: patient waiting times, number of patients treated, and financial result. Among the 35 suggestions that we originally collected from the project team, we were able to isolate two key leverage points: reducing treatment times in the critical care and telemetry units and improving the shared nursing arrangements among three departments to increase their ability to meet surges in demand.
Initial Outcomes
Shifting the Burden of Emergency Care
Our SJ MC team completed the systems thinking project in the summer of 1990. Since then, on the joint initiative of the Hospital Conference of Santa Clara County (which included SJMC representatives), the County , Medical Society, and the County Emergency Medical Services Agency, the San Jose community implemented a public policy that maintains an “open” emergency status at all of the community’s hospitals. Although it is still too early to evaluate the long-term results, the diversion rate virtually disappeared in the initial months. In light of the systems “rule of thumb” that quick fixes do not produce lasting results, we expect diversion problems may creep back up during the coming months. Over time, we may need to refine the public policy approach so that long-term adjustments are made and the system is restored to balance. In addition to working on the community-wide capacity problems, at SJMC we are currently using the insights gained from the computer model to develop strategies for improving our internal capacity.
Bette Gardner is a healthcare management consultant in Morgan Hill, California. She is applying systems thinking in her work at San Jose Medical Center and elsewhere.