According to the World Health Organization, vaccines and clean water are the two public-health interventions that have had the greatest impact on the world’s health. In the U.S., vaccination programs have played an important role in virtually eliminating serious diseases such as diphtheria, whooping cough, polio, and measles. And vaccines aren’t just for kids anymore—immunizations against flu and pneumonia save adult lives as well. But distrust of immunization programs is on the rise. As William Schaffner, M. D., chairman of the Department of Preventive Medicine at Vanderbilt University, says in the Consumer Reports article, “We’re prisoners of our own success. When formerly dreaded diseases have been pushed into the shadows—or eliminated—questions about the vaccines themselves spring up.”
Weighing the Risk
In recent years, groups that oppose vaccinations because of their potential health risks have sprung up. For instance, some activists claim that the mumps, measles, rubella vaccine is linked to autism, although medical groups studying the possible connection have concluded that the vaccine is not to blame. Anti-immunization groups also doubt the government’s ability to oversee vaccine safety, pointing to, among other things, its delay in banning mercury from injections, despite the fact that it can impair children’s cognitive development.
In response to such concerns, more and more people are choosing not to vaccinate. When weighing the risk of contracting vaccine-preventable diseases against that of experiencing one of the rare catastrophic reactions to the vaccine itself, they are banking on current low levels of infection and deciding to avoid the injections.
Health officials acknowledge that vaccines can cause side effects, ranging from mild (temporary pain at the injection site) to serious (between 1960 to 1999, 8 to 10 children a year in the U. S. contracted paralytic polio from the oral polio vaccine).
But they also point out that as more people avoid immunization, the incidence of certain serious diseases is bound to rise. As just one example, the Consumer Reports article cites the case of Mary Catherine Walther, who contracted Hib meningitis on her first birthday. Her local hospital in Tennessee hadn’t treated a case of the illness for eight years, since the introduction of a vaccine against it. Fortunately, the toddler recovered.
THE SWING OF RELATIVE RISK
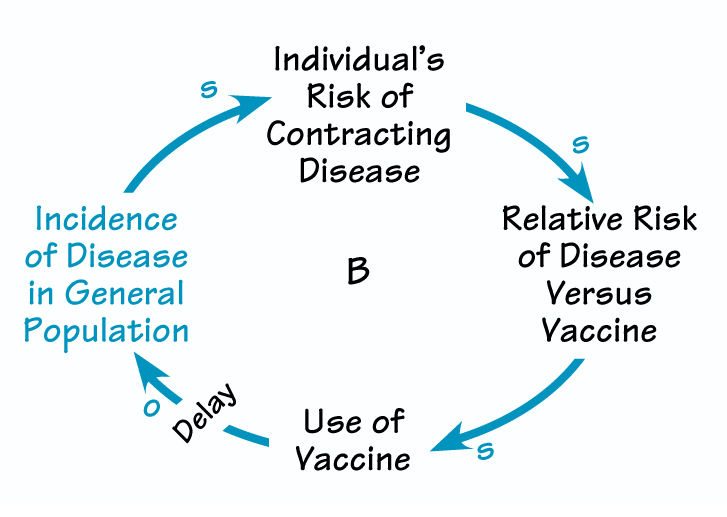
As the incidence of a disease rises, people’s perception of the risk to their own health increases. Under these conditions, they are more likely to overlook the vaccine’s side effects. Use of the vaccine reduces the incidence of the disease. When infection rates fall, people’s concerns about vaccine safety grow. If enough people choose not to use the vaccine, the disease begins to spread again.
One reason that formerly dormant diseases can reappear is that they haven’t yet been eradicated worldwide. Travelers from countries where immunization programs have been limited can carry a disease to other regions. Or such illnesses could reemerge through more diabolical means. In June, a simulation exercise depicted a smallpox attack by terrorists that infected 24 people in Oklahoma. After an imaginary two weeks, 16,000 people in 25 states were infected; 1,000 were dead; and 10 other countries reported cases. Following these trends, within three weeks, there would be 300,000 victims, a third of whom would die. Without continued vigilance, such an epidemic could also happen with other serious illnesses that we have long thought were cured.
Relative Risk
The pendulum swing between concerns about disease to concerns about the vaccines themselves represents a classic balancing process (see “The Swing of Relative Risk”). When the threat of a specific disease is high, the vaccine’s desirability rises, regardless of safety concerns. When incidences of the disease are few and far between, people start raising questions about the vaccine’s side effects.
Rather than writing off such concerns as irrational, by recognizing this dynamic, public-health officials can anticipate and manage them through ongoing investments in vaccine safety, education, and immunization programs around the world. In fact, officials might consider activists’ skepticism to be a positive force, in that it keeps pressure on manufacturers and governmental agencies to continually improve these life-saving products. After all, no one wants the cure to be worse than the sickness.
Janice Molloy is managing editor of The Systems Thinker.