“Medical cost cutters known as utilization review companies…have become immensely popular with employers seeking to control their health-care costs…[D]oubt is growing about the new industry’s most basic promises — lower medical costs…For every form a utilization firm sends out and every phone call one of its employees makes, someone in the medical community must respond, usually with equal or greater effort…To some industry specialists, the issue embodies a Catch-22 of medical economics: Efforts to police costs add to the industry’s administrative burden.” (“Firms that Promise Lower Medical Bills May Increase Them,” The Wall Street Journal, July 28, 1992)
* * * *
Utilization review (UR) procedures have become common in healthcare, as employers try to manage costs by restricting and limiting unnecessary care. For a while, such procedures worked: a study in Medical Care that analyzed 223 insured groups from 1984 to 1986 concluded that hospital admissions decreased 13% and overall medical costs were cut 6%, as a result of UR.
But The Wall Street Journal article raises concerns about the overall financial benefits of these procedures, be-cause of the great administrative burden they place on doctors and hospitals. Some analysts estimate that 20% of the current healthcare bill can be attributed to excess paperwork and other administrative-related tasks. By the year 2020, such spending could amount to half of total healthcare dollars. Although the UR system worked well at cutting costs at first, recent problems and increased administrative costs for providers suggest that the UR industry is suffering from a “Fixes that Fail” situation.
The Utilization Review Fix that Failed
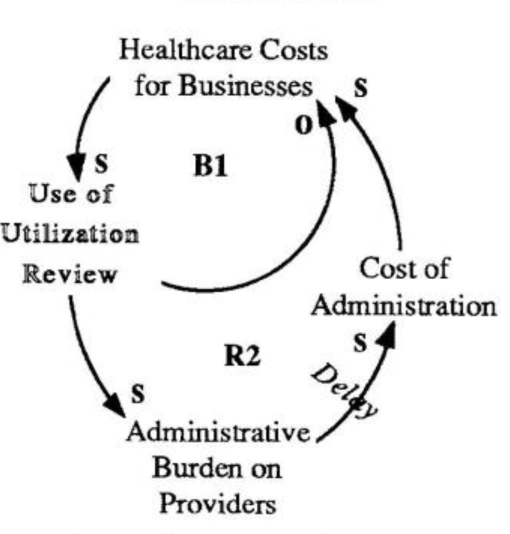
As healthcare costs skyrocket, utilization review helps businesses reduce their spending (81). Over time, however, the additional administrative burden on providers caused by UR leads to higher costs, which are eventually shifted back to the employer (RI ).
Some generic structures occur so frequently that they have been identified as a generic set of tools called “systems archetypes.” This column is designed to help readers recognize archetypes at work in newspaper and magazine articles.
UR is popular because the cost savings far outweigh the fees charged to employers (B1 in “The Utilization Review Fix that Failed”). But over the long term, the increased costs to providers will lead to increased costs of services, further cost-shifting to patients, and in the end, greater costs for employers (RI). The increased costs are invisible for the most part, since the extra time it takes to answer a phone call or chase down information for a report is not measured.
Clearly, UR firms have helped employers deal with their biggest concern with healthcare: increasing costs. But the “Fixes that Fail” archetype suggests that any successes will be short-lived. As the healthcare system is revamped, it is critical that employers and providers focus on the long term and make sure any proposed “fixes” will not worsen the healthcare crisis (see “No More Band-Aids for Health-care Reform,” Cover Story, August 1992).(‘The Systems Thinker’ 4 Vol. 3, No. 7 01992 Pegasus Communications, Cambridge, MA)