Microtown, a small community deep within the Land of Middle Health, isn’t much different from other towns. Its citizens are young and old, rich and poor, employed and unemployed. Some come from large families; others live alone.
Up until a year ago, Microtown’s healthcare system wasn’t much different, either. Although most of the system was operating with a high degree of efficiency — surgeries and procedures were performed on schedule, and x-rays and lab tests were completed at small per-unit costs — these improvements had not yielded significant benefits in terms of the overall health of the community.
Then one day last year, a dramatic event occurred. In a blinding flash, Microtown’s healthcare system was completely dissolved. All the “hard” assets — the bricks and mortar, the technology and infrastructure — were converted into cash. The “soft” assets — the people in the system — were left with their abilities and expertise still intact. But their mental models, which had limited their ability to envision an alternative future, were wiped out entirely.
An Idealized Design
After the people of Microtown recovered from their initial shock, they were confused about how to design a new healthcare system. However, they recognized that they had been given a unique opportunity to create an innovative, long-term approach to healthcare — an idealized design, if you will. The parameters were simple: whatever healthcare system they designed had to use existing technology and be sustainable.
With these objectives in mind, Microtown’s citizens and healthcare professionals got to work. They first worked on redefining “healthcare” as a continuous loop of learning and clinical service, beginning before birth and culminating in hospice care at the end of life. From this perspective, they recognized that a key element of their new design should focus on managing care, with an emphasis on keeping people healthy and happy. They developed new incentive systems by paying for early intervention services and rewarding community efforts to educate citizens about healthy behavior. They also worked to incorporate patients into the system as partners, by giving them the opportunity to voice their recommendations and concerns and thus contribute to the overall design process.
Finally, the citizens of Microtown decided to dedicate themselves to applying systems thinking and quality management principles to their healthcare redesign efforts. Together, they committed to:
- understanding and respecting the community as a whole
- integrating more fully all of the systems involved
- building a shared vision of healthcare
- creating and sustaining a process of continuous improvement in healthcare delivery
In addition, they endeavored to make tools, techniques, and processes available to facilitate learning, improve quality, and provide safe containers for dialogue.
Slowly, a new excitement began to grow within the community of Microtown. Over time, schools, churches, families, and community associations became active in addressing the broader health issues that affected their lives, such as diet, nutrition, exercise, safety, and community violence. They supported new educational and community programs that nurtured family life in the town. And more importantly, they saw the need to work toward a more seamless continuum of services that included partnering resources for patients who required more intensive care.
The enthusiasm in Microtown continued to build as people recognized how a healthcare system that leverages prevention and early intervention — and is built on a belief in individual empowerment and group collaboration — can result in enhanced community health. They saw how an improvement in the health status of citizens could translate into increased productivity for the community as a whole, enlarging the resource base available for the community’s continued growth and development (see R2 in “Community Impact of Improved Health”). Overall, Microtown’s efforts to create a new healthcare system were viewed as a way to strengthen the entire community through shared participation and increased integration of each of the community’s systems.
Community Impact of Improved Health
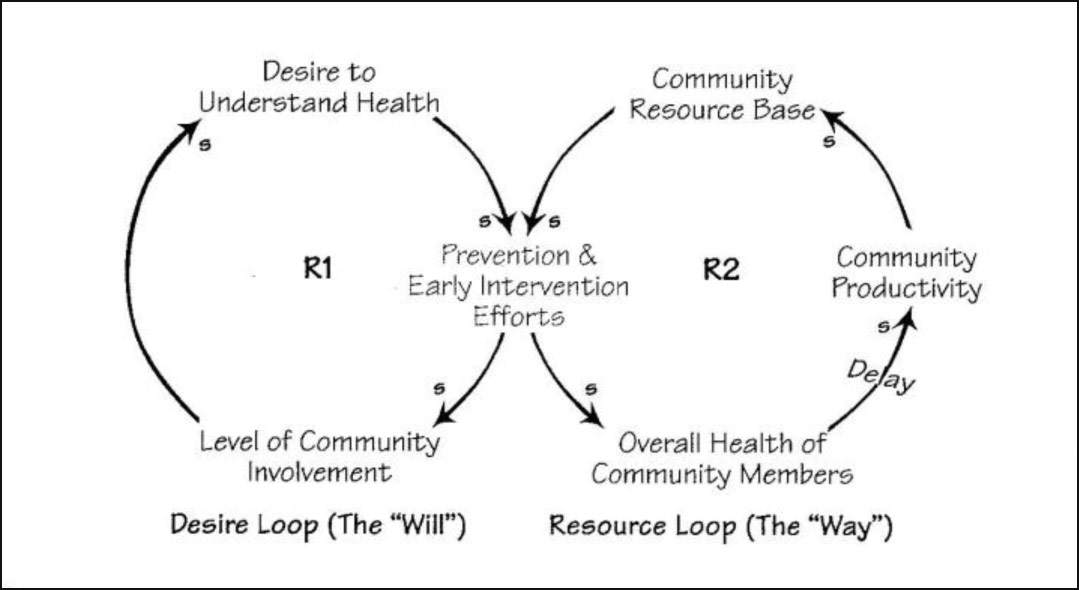
People In Microtown recognized that a focus on prevention within their community would lead to an increased sense of ownership and responsibility (RI ). And as their community helped people to better understand health issues, they could leverage prevention and early intervention to improve health and enhance long-term community productivity (R2).
Healthcare vs. “Sickcare”
Clearly, Microtown’s experience is a fictional scenario. In the real world, the systems that impact healthcare are much more complex, the solutions less obvious, and the mental models of past systems are always present. But it is still possible that tools like idealized design, systems thinking, dialogue, and shared vision can be used to accelerate community learning. What would happen if healthcare issues were reframed in a larger, more systemic context? What if time were spent creating a shared vision of improved community health? Could a higher quality healthcare system — one that would be of greater value to the community — emerge from such a process?
If the current U.S. healthcare system continues to operate as it has in the past, it will remain out of sync with the needs of our communities. In the present system, resources are heavily concentrated at the latter stages of the disease process (in part because the largest profits are made when the patients’ needs are the most acute). This has led to an emphasis on treating the sick and severely ill, rather than a focus on disease prevention. Providers and administrators are only now beginning to realize that it is more cost effective to provide proper disease prevention than to focus primarily on treating patients at the latter stages of disease.
In order to create long-term, systemic change, we must address the incentive systems that have helped create the current healthcare crisis: (1) health insurers tend to cover only healthy people, leaving the elderly and the ill without resources; (2) physicians are paid on a fee-for-service basis to “do more,” and are not financially motivated to intervene early; and (3) hospitals are driven by economic need to increase admissions and occupancy by drawing large volumes of people to their doors.
These incentives almost always run counter to the patient’s preference to be well, healthy, and independent. They also run counter to the overall efficiency of the system, which argues for early intervention in any disease process. There is little debate that what we call a “healthcare” system is, in reality, a misnomer. A more appropriate term would be a “sickcare” system.
A System Model of Health
In a redesigned healthcare system, resources including facilities, programs, and technologies would be integrated with human capability to manage the flow of patients into — as well as within — the healthcare system (see “Redesigned Healthcare System”). But the new system would need to go beyond the current quality improvement efforts, which are targeted at reducing costs and improving outcomes for people who are already in some phase of intervention (RI and R2). It should also focus on reducing the rate of illness (via preventive care) and increasing access to the system of care, because this is where the greater leverage for improved care lies.
This means taking the financial resources gained through cost reductions and investing those funds in institutional capacity to expand access and increase preventive care. Increasing preventive care creates a virtuous loop of cost savings via reducing illness: by decreasing the rate of illness, we can lower the number of patients in intervention, which lowers costs and increases financial resources, which can then be invested in more preventive care (R3). In addition, investments made in contracting can expand access to the system of care, which increases the number of people participating in healthcare policies. This will lead to more revenues and thus to more financial resources to invest in both contracting and preventive care (R4).
Redesigned Healthcare System
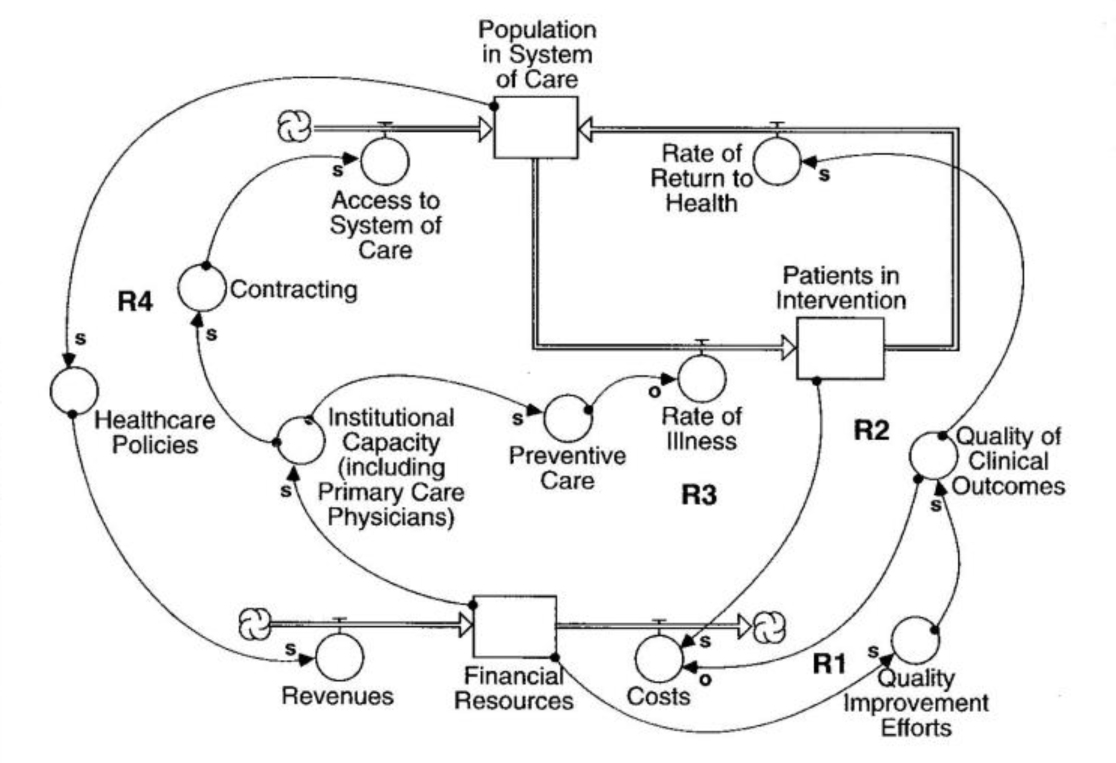
One point of high leverage for improving healthcare is managing the flow of patients in need of care. As this accumulator and flow diagram illustrates, focusing on reducing the rate of illness through preventive care lowers the number of patients in intervention. This lowers costs and increases financial resources. Which can then be invested in more preventive care (R3). In this system, healthcare resources are directed toward high efficiency and quality, and toward patients flowing back into the healthy population.
A system that emphasizes the positive reinforcing nature of loops R3 and R4 shifts the emphasis from increasing interventions to increasing health, and it shifts the focus from limiting access to maximizing access. But partnership is required to create this kind of system. Those charged with clinical outcome accountability and those shepherding the system’s financial resources must have aligned incentives in order for the system to work well. In addition, everyone who influences the system must be committed to a shared vision of what is possible and how the needs of various stakeholders can be balanced for the good of the system.
It is important that each stake-holder plays a role in the creation of healthcare policy. For example, educating patients about the healthcare system as a whole will enable them to become informed consumers of healthcare, gaining knowledge about their own needs and choosing efficient, low-cost ways to meet those needs. In addition, physicians need to learn to manage care by emphasizing early intervention and the management of disease. Finally, physicians and providers must ensure that there is an adequate distribution of access to primary and preventive care for patients, as it will impact the clinical needs of the patients who come to them.
Community Case Management Programs
A community case management program provides a systematic approach for assessment, planning, service, and referral that identifies and meets patients’ needs. When case managers follow their patients closely, they are able to discover problems that may have otherwise remained hidden and quickly help to remedy them.
In Baton Rouge, for example, a patient with congestive heart failure, who lived alone in a second-floor apartment, began to notice some swelling in his feet. When the case manager called to see how his patient was doing, he discovered the source of the problem: the man had stopped raking his medicine (which controlled his fluid volumes but also caused him to urinate frequently) because his toilet was broken. The plumber wasn’t coming for two days and he didn’t want to keep bothering his neighbor by using her bathroom. The case manager arranged for a bedside commode to be delivered and instructed the patient to resume his medication immediately. He then scheduled a follow-up appointment with the patient’s doctor, averting the probability of a hospital re-admittance because of a worsening heart condition.
Through this type of case management program, we have reduced patient re-admission rates for General Health System from 88% to 33%.
How One Community Is Responding
What happened in the fictional Microtown is slowly happening in communities throughout the U.S. Some clinical program areas are being redesigned from an outcomes perspective. Organizations of providers are working to align incentives to provide more efficient and effective care under a collaborative model. Insurers are reconsidering their responsibility to their constituents. Key components of health systems are “unfreezing” themselves and readying for change.
For example, at General Health System in Baton Rouge, Louisiana, we have been working for the last three-and-a-half years to apply the tools of systems thinking, idealized design, and dialogue to create a more effective healthcare system. One of our goals is to provide community members with a continuum of care, beginning with primary care and community health education and outreach programs. Using these programs, our patients are learning how to take care of their bumps, bruises, and simple fevers themselves. They are encouraged to participate in programs to stop smoking, improve their diets, and increase their physical strength, endurance, and flexibility. Primary care physicians, well-baby clinics, school health, and jobsite clinics provide members throughout the community with health screenings and knowledge about their current health status, as well as appropriate actions for maintaining good health.
Baton Rouge community case management programs also help people manage illness when it does occur (see “Community Case Management Programs”). Ambulatory services, including x-rays and lab tests, provide support services that give patients a greater understanding of the status of their health, enabling them to maintain some control over the treatment process while under the supervision of their doctors. For those who require acute care in hospitals, case managers and nurse specialists provide restorative care as their conditions improve — helping patients return home and minimizing their chances of re-admittance to the hospital. Intensive-care units and treatment centers provide lifesaving care to those with serious illnesses, but the purpose of intensive care is always to return the patient to a level of health that can be managed at home, maximizing the patient’s independence. Home-care programs provide support to those recuperating at home, as well as those in need of long-term care. In addition, hospice care, social services, and support groups are offered to patients and their families at the end of life’s journey.
With this kind of system in place, we believe that community health providers will be better able to track and predict disease occurrence in the community and to collaborate on the best ways to decrease illness through prevention. Our hope is that, once the effectiveness of working in a partnership is demonstrated, the groups will become motivated to plan together for early intervention, for treatment when necessary, and for long-term, clinical follow-up to ensure maximum health for patients.
Learning and Results
A major lesson from our redesign efforts at Baton Rouge is the importance of emphasizing primary and preventive care. Rather than use resources for intensive-care centers, for example, those funds can be more effectively allocated to prevention programs. In addition, the “best practice” process can contribute to the focus on preventive care. Once a specific desired outcome and a set of shared values are clear, players can map the best practice process for achieving that outcome. For example, in the best practice treatment of asthma, everyone in the system — schools, employers, healthcare providers, and patients — collaborates in preventing asthma, thus reducing the number of patients who end up in emergency rooms as a result of acute asthma attacks (see “A Systems Approach to Asthma Treatment”).
Once a desired outcome is mapped, it is easier to determine objectively if a variation from the map is appropriate. The best practice guideline can then be altered to fit the unique needs of each patient. Once the creativity of individuals is focused on a desired goal, rather than on defending the status quo, innovation and improvement will increase.
Changing Mental Models
Managing the transition to a new healthcare system will be challenging. However, new and powerful management tools such as dialogue can assist in this process. With a genuine intent to understand one another, individuals and groups with varied agendas can come together, work through differences in perception, and learn how those differences create conflicting “realities” and negative mental models.
It takes time to create shared values and vision. But once the group develops a shared understanding and commitment to a common future, they can begin the technical process of clinical care reengineering. Time spent on creating a commonly held definition of “health,” as well as on how to measure and value it, will reap huge dividends when making decisions on prioritizing outcomes of the health system.
There are, however, risks to be avoided in this process of creating a new system. While today’s industry pressures emphasize cost above all else, redesigned models cannot be measured purely by financial performance. Fiduciary accountability must be balanced with the less tangible benefit of improved health throughout the community. In other words, the system will operate at optimum performance when all costs — good financial figures and the well-being of humans — are taken into equal account. The real measure of a successful healthcare redesign will be the growing number of knowledgeable consumers who will accept nothing less than a balanced system that works to the benefit of all involved.
Shelly Bright is senior vice president for strategy and organizational development at the General Health System in Baton Rouge, LA.
Gene Beyt. M.D., Is senior vice president of medical affairs for the system. Together, they work with General Health’s senior leadership to transform the system and to provide community benefit.
Editorial support for this article was provided by Virginia O’Brien.
A Systems Approach to Asthma Treatment
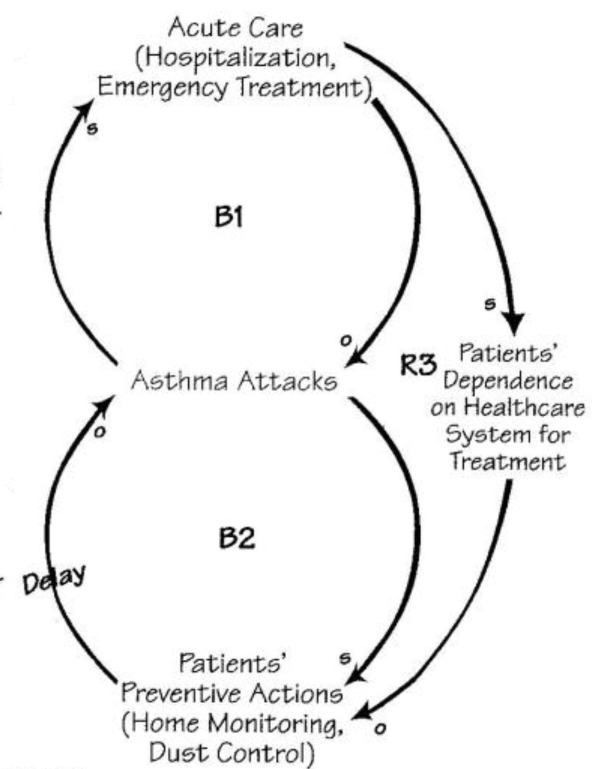
Today’s treatment for asthma patients illustrates the current fragmented approach to many common health problems. During asthma attacks, patients wheeze, cough, and experience shortness of breath. When experiencing these symptoms, they often require intravenous fluids and medications, which are frequently administered in an emergency room (B1). This medical intervention results in frequent hospitalizations, loss of school Acute Care and work time, and accompanying costs. Over time, these interventions shift the burden of responsibility from the individual to the “acute care” system. This increased dependence on acute care increases costs throughout the system and takes away patients’ control over their own health (R3).
A “best practice” treatment of asthma, which drives this “Shifting the Burden” structure in reverse, demonstrates the efficiency and better quality of care that could result from a redesigned system. D2 In this case, asthmatic patients are considered partners. They measure their respiratory function at home and use preventive medicines (B2). With home therapy, the patient is able to intervene early — as soon as he or she notices changes in respiratory functions — thus reducing the need for emergency treatment. Other care as simple as controlling dust in work and school environments provides healthier air and decreases asthmatics’ exposure to offending agents that trigger symptoms. Patients thus become less dependent on the system and gain greater control over their health problems. With an improved quality of life and a system based on prevention, illness-related expenses throughout the system are contained.